Kavitha Kothapally1*, Uma Bhashyakarla2, Tilak Chandrapal3
1, 2Dept. of Obstetrics & Gynaecology, Bhaskar Medical College & General Hospital, Yenkapally, Moinabad, Rangareddy–500075, AP, India.
3Dept. of Paediatrics, Bhaskar Medical College & General Hospital, Yenkapally, Moinabad, Rangareddy–500075, AP, India.
ORIGINAL RESEARCH ARTICLE
ARTICLE INFORMATION
Article history
Received: 16 December 2013
Revised: 26 December 2013
Accepted: 29 December 2013
Early view: 30 December 2013
*Author for correspondence
E-mail: [email protected]
Keywords:
Spontaneous multifetal pregnancies
Complications
Mode of delivery.
Background: The present study was done at Bhaskar General Hospital, a teaching hospital located in a rural area in AP. The aim of the study was to analyze the occurrence of spontaneous twinning among the rural pregnant women attending this hospital.
Subject and Methods: The study was conducted from January 2011 to December 2013. The study showed the incidence of spontaneous twinning as 1.3 per cent of births at our hospital.
Result: A total of 40 cases of spontaneous twins were noted over 3 year observation periods. More than 80% were multigravidae & 20% were primigravidae. 5% had treatment for infertility. 12.5% had family history of twins. 80% were in the age group of 21-30 yrs. 80% were dichorionic diamniotic twins. Most of them could be delivered after 34 wks with live fetuses weighing more than 2 kg birth weights with minimal complications of mother & child.
Conclusion: Incidence of spontaneous twinning was 3.8% in the studied population. Most of the pregnant women in the study population did not have any etiology. Negligible number had twinning after treatment for infertility. With adequate bed rest, early hospitalization at 32-34 weeks with careful monitoring by NST & USG, nearly all patients could continue their pregnancies beyond 36 weeks of gestation. Regarding mode of delivery, the guidelines are based on presentation, fetal weight & fetal well being. Well known complications included abortion, hyperemesis, anemia, PIH, IUGR, preterm labour, PROM. Others are malpresentations, abnormal lie, polyhydramnios, PPH, retained II twin & increased operative vaginal delivery.
INTRODUCTION
Incidence of twinning is greatest among blacks, least common in Asians & of intermediate occurrence in whites (Martin et al., 2006; ACOG 2004). Incidence of twins is 12/1000 births in U.S, 49-53/1000births in Africa & 3% of all births on an average (Martin et al., 2006; Obiechina et al., 2011). A place called Yoruba has the highest rate of twinning (45-50 twin sets /1000births).This is attributed to the high consumption of a special type of yam containing a natural phytoestrogen which may stimulate the ovaries to release ova from both ovaries. A high incidence of twinning is seen in Kodinji in India. Women who have a family history of fraternal twins have a higher chance of producing fraternal twins themselves as there is a genetically linked tendency to hyperovulate. Other factors that increase the odds of having fraternal twins include maternal age, fertility drugs & other fertility treatments, nutrition & previous births. Recent studies showed that insulin-like growth factor present in dairy products may increase the chance of dizygotic twinning. Genotypes favouring elevated insulin like growth factor & diets including dairy products especially in areas where growth hormone is given to cattle appear to enhance the chances of multiple pregnancies due to ovarian hyper-stimulation. Other causes could be increased growth hormone in food. Incidence of twinning in ART & ovulation induction comprises 25-30% of all deliveries resulting from ARTs. Other factors are family history of twins especially in a first degree relative on maternal side, easy conception within 3months of marriage & pregnancy soon after cessation of long term oral contraceptives (Pernoll et al., 2003; Luke et al., 2004).
Mean age of mothers - 28.4yrs. Mean parity is two. Vertex- nonvertex presentation occurs in approximately 40% of all twins. Some favour elective caesarean section to minimize the risk of fetal trauma and asphyxia (Kelsiek et al., 1982). Mean gestational age at which twins are delivered is 34wks +/-5.2wks. Mean birth weights were 2.3-3.14kg+/-1 kg. Elective hospitalization for bedrest, prophylactic tocolytics, use of cervical cerclage are measures proposed to reduce fetal wastage through prterm labour but have not shown benefit practically. Maternal nutritional intervention has emerged as the only means of improving outcomes in twins(Hogle et al .,2008).Well known complications include abortion, hyperemesis, congenital malformations, anaemia, PIH, IUGR, Preterm labour, PROM, APH(ASPM 2008). Others are malpresentations, abnormal lie, polyhydramnios, cord prolapse, cord entanglement, UTI, PPH, retained II twin & increased operative vaginal delivery (Sentilhes et al., 2009; Barrett et al., 2002; Webster et al., 2011; Ilesanmi et al., 2000; Owen et al., 1997). HTN, cord prolapse, malpresentations, PROM, low apgar scores, increased caesarian section rate, increased perinatal deaths are high in twin pregnancies.
Route of delivery of twins should be determined by position of fetuses, FHR monitoring & maternal & fetal status (ACOG 2004). Active second stage management in normal delivery is associated with neonatal outcomes similar to those with planned cesarean delivery (Ahmed et al., 2013). External cephalic version & internal podalic version require expertise & have success rates of 45% & 97%, respectively (Sentilhes et al., 2009; Barrett et al., 2002). Though maternal risks remain the same, fetal risks are 18% more with external cephalic version & 1% more with internal podalic version (Webster et al., 2011).
SUBJECTS AND METHODOLOGY
Ethical consideration
After obtaining the approval of the Institutional Ethics Committee, the study was carried out between January, 2011 and December, 2013. The study was done at Bhaskar Medical College & General Hospital, Andhra Pradesh in the Department of Obstetrics & Gynecology. Out of 1080 deliveries that occurred over 3 years at Bhaskar Hospital, 40 cases of twin pregnancies were registered over 3 years of study period. Details of patient like -age, address, parity, regularity of menstrual cycles, history of treatment for infertility, family history of twins, consanguinity, past history of twins & gestational age at which twins were diagnosed first were noted. Twin pregnancies were followed antenatally for the development of any complications. Mode of delivery, birth weights of newborns, and any postpartum complications were also noted.
RESULT
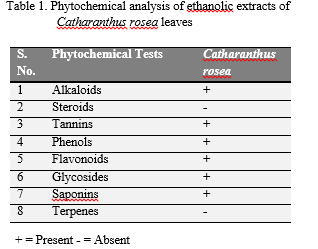 |
Table 1 Age distribution. Click here to view full image |
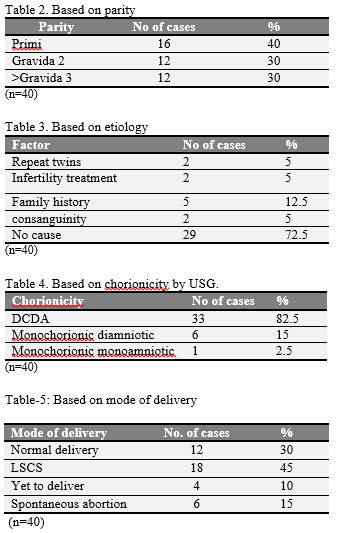 |
Table 2-5 Based on parity,etiology ,chorionicity(by USG)and delivery respectively. Click here to view full image |
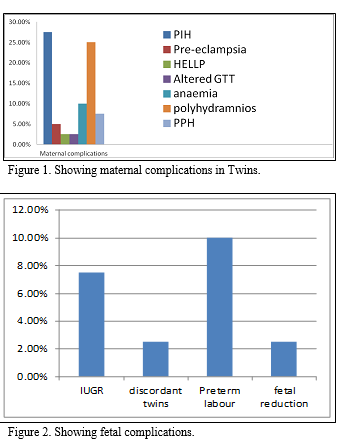 |
Figure 1-2 Showing maternal complications in Twins and fetal complications respectively. Click here to view full image |
DISCUSSION
Multiple pregnancy is always an interesting scientific occurrence. Since the increased use of IVF techniques, its incidence has increased .In our study we observed that multiple pregnancies occurred without any such iatrogenic interventions in the rural population of RangaReddy district,AP. From tables 1 & 2 we see that the common age group was between 21-30yrs & more than 80% were multiparous. As per the table 3, about 12.5% of women had family history of twins & 5% had consanguinity. 5% took treatment for infertility. 72% had spontaneous twinning. About 40 % were diagnosed in the I trimester & 60 % were diagnosed in the 5th month.From the graph 1, Complications like PIH(20%), preeclampsia (4%), HELLP syndrome(2%),altered GTT(2%), Polyhydramnios(20%), PPH(4% %) , anemia (8%) were observed in the studied population.IUGR was seen in 6% & discordant twins in 2% . One patient had spontaneous triplets and went for fetal reduction. Adequate bedrest, early hospitalization around 32-34 wks of gestation allowed the pregnancies to continue beyond 36 weeks with FHR monitoring by NST. From the table 4, we see that 30% had normal delivery. 40% had LSCS for various obstetrical indications.6 cases are yet to deliver & 6 had spontaneous abortion. Dichorionicdiamniotic placenta is seen in 50%, monochorionic placenta in 15% & monochorionicmonoamniotic placenta in 3% of the cases. Delivery time interval between both twins in normal delivery was 10-20 minutes on an average(Obisesan et al.,1999). Ist twin presented as cephalic in 76.6% of cases, 23% were breech & 2.5% presented as transverse lie as per the graph 3. As we observe in graph 4, fetal weights were less than 2kg in 26.6% of cases, 2-2.5kg in 46.6% of cases, 2.5-3kg in 20% of cases & more than 3kg in 6.6% of cases.
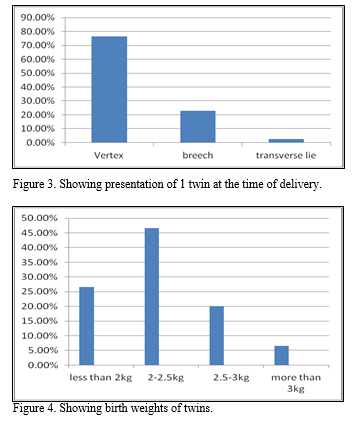 |
Figure 3-4Showing presentation of 1 twin at the time of delivery and birth weights of twins respectively. Click here to view full image |
CONCLUSION
Incidence of spontaneous twinning was 3.8% in the studied population. Incidence of twins was 30.6/1000 births in a study in Nigeria. Most of the pregnant women in the study population did not have any aetiology. Negligible number had twinning after treatment for infertility. Their dietary habits & environmental factors have to be studied to analyze any of their effects on twinning in the region of the studied population. With adequate bed rest, early hospitalization at 32-34 weeks with careful monitoring by NST & USG, nearly all patients could continue their pregnancies beyond 36 weeks of gestation. Regarding mode of delivery, the guidelines are based on presentation, fetal weight & fetal well being. Well known complications included abortion, hyperemesis, anemia, PIH, IUGR, preterm labour, PROM. Others are malpresentations, abnormal lie, polyhydramnios, PPH, retained II twin & increased operative vaginal delivery.
REFERENCES
ACOG committee on practical Bulletins—Obstetrics Society for maternal fetal medicine, ACOG Joint Editorial Committee authors, ACOG Practice Bulletin No. 56, multiple gestation: Complicated twins,triplet & high order multifetal pregnancy. Obst Gynaecol.104, 869-883, 2004.
Farhatulain Ahmed, Noorikiran Naeem, Shamila Yasir, Management of Nonvertex Second Twin. J Obstet Gynecol India. 63, 177-181, 2013
American society for Reproductive Medicine, Patient’s fact sheet, complications of multiple gestation,2008, http://www.asrm.org/Complications_and_Problems_associated_with_Multiple_Births/, accessed on 15 July, 2012.
Barrett JF, Ritchie WK. Twin delivery. Best Pract Res Clin Obstet Gynaecol. 16, 43-56, 2002.
Hogle KI, Hutton EK, Mebrian KA, Baret JF, Hannah ME,cesarean delivery for twins: A systematic review & meta analysis. Am J Obst Gynaecol. 88, 220-227, 2008.
Ilesanmi AO, Obisesanka, Arowojulu AD, Fawole O, Roberts AO, Relative birth weights in twins. Nigerian Medical J, 38, 14-15, 2000.
Kelsiek F, Minkoff H. Management of Breech second twin. Am J Obs & Gyn.144, 783-786, 1982.
Luke B, Improving multiple pregnancy outcomes with nutritional interventions. Clin Obst Gynaecol. 47, 146-162, 2004.
Martin JA, Hamilton BF, Sutton PD. Births: final data for 2004, National Vital Statistics Reproduction (NVSS). 55, pp 1-101, 2006.
Obiechina NJ, O Kolie VE, Eleja GU,O Kechukwu ZE, Anemaja OA. Twin verses singleton pregnancies: the incidence, pregnancy complications & obstetric outcomes in a Nigerian tertiary hospital. Int J Women’s Health. 227-230, 2011.
Owen P. Twin pregency. British J Hospital Med. 58, 437-439, 1997.
Pernoll ML, Melissa M. Multiple pregnancy, In Decherney DH, Pernoll ML, editors. Current obstetrics & gynaecologic diagnois & treatment 9th edition, New York, NY: McGraw Hill & Lange Medical Books, 2003.
Sentilhes L, Bouhours AC, Biquard F, Gillard P, Descamps P, Kayem G. Delivery of twins. Gynecol Obstet Fertil. 2009 37, 432-41.
Webster SNE, Loughney AD. Internal podalic version with breech extraction. Obst Gynaec. 13, 7-14, 2011.




 This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.