Muhammad Uwais Ashraf1, Mohd Aslam1*, Masihur Rehman Ajmal1, Anwar Habib2
1Department of Medicine, JN Medical College, AMU Aligarh, UP, India.
2Department of Medicine, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard. New Delhi, India.
ORIGINAL RESEARCH ARTICLE
Volume 2, Issue 3, Page 131-135, September-December 2014.
Article history
Received: 25 November 2014
Revised: 15 December 2014
Accepted: 20 December 2014
Early view: 30 December 2014
*Author for correspondence
E-mail: [email protected]
Mob: +918755079729
Introduction: Elevated level of plasma homocysteine has been demonstrated to be an independent risk factor for the development of coronary artery disease. The effects of plasma homocysteine have been demonstrated to be due to its highly atherogenic and prothrombotic properties. The current study aims to establish the association between elevated homocysteine level and the extent of myocardial injury measured by cardiac troponin-I and ejection fraction in patients admitted with acute coronary syndrome.
Subjects and Methods: This was a cross sectional, open labeled, hospital based study conducted on 200 patients admitted with acute coronary syndrome in the coronary care unit of J N Medical College, AMU, Aligarh, India, during October, 2013 to November, 2014. Informed consent was taken from all patients. A detailed history was taken and a thorough clinical examination was carried out. Cardiac troponin- I (cTI) was measured after 10 to 12 hours of onset of symptoms. Echocardiography was carried out in all patients.
Results: Of the patients with ACS, 62 (31%) had unstable angina, 52 (26%) had NSTEMI and 86 (43%) had STEMI. The mean homocysteine level of the study population was 37.65±12.8 μmol/L. Significant positive correlation was found between Serum Troponin-I level and homocysteine level (P<0.001). Also, a positive correlation was found between serum homocysteine levels and ejection fraction. The R square for this relationship was 0.244, with a p value of <0.001.
Conclusion: Serum homocysteine is associated with increased myocardial injury which has been quantified in the current study by serum cardiac troponin-I levels and ejection fraction, which are independent markers of the extent of myocardial damage in patients of acute coronary syndrome.
Keywords: Homocysteine, troponin, acute coronary syndrome.
INTRODUCTION
Homocysteine (Hcy) is an amino acid which is an important intermediary compound in the metabolism of methionine. This pathway leads to the formation of methionine and cystathionine and is regulated by various enzymes like Vitamin B12, B6 and Folic acid. Abnormality in any of these enzymes or deficiency of either of these vitamins may give rise to hyperhomocysteinemia. Hyperhomocysteinemia has been classified as: Moderate (Hcy >15 to 30 μmol/L), Intermediate (Hcy >30 to 100 .μmol/L) and Severe (Hcy >100 μmol/L).
Elevated level of plasma homocysteine has been demonstrated to be an independent risk factor for the development of coronary artery disease (Clarke et al., 1991). The effects of plasma homocysteine have been demonstrated to be due to its highly atherogenic and prothrombotic properties (Harker et al., 1976). It has been shown by previous studies that patients who have angiographically determined coronary artery disease have an increase in the risk of death with increasing homocysteine concentrations (Nygard et al., 1997). Previous studies have reported an association between homocysteine concentrations and plasma markers of thrombosis activation in patients admitted for acute coronary syndrome (Al-Obaid et al., 2000). These findings have postulated that elevated homocysteine concentrations lead to increased myocardial injury in acute coronary syndrome and thus lead to worse prognosis of acute coronary syndrome.
The exact mechanism of atherothrombosis due to hyperhomocysteinemia has not been clearly defined and understood. However, previous studies have hinted towards an association with inhibition of thormbomodulin activity, reduction of protein-C activation, increased platelet aggregation, and predisposition to endothelial injury secondary to hyperhomocysteinemia. Also, hyperhomocysteinemia leads to proliferation of smooth muscle, it increases the oxidation of LDL cholesterol, and induces proinflammatory changes in the vessel walls (Hayashi et al., 1992).
Few previous studies have shown an association between homocysteine concentration and plasma markers of thrombosis activation in patients presenting with Acute Coronary Syndrome (ACS) (Al-Obaidi et al., 2000). Cardiac Troponin-I, which is specific for cardiac tissue, is detected in the serum after myocardial injury has occurred. Serum troponin-I level has been shown to reflect the extent of myocardial injury in acute coronary syndrome (Eric et al., 2000). Therefore, levels of serum troponin correlate with the extent of myocardial damage.
Similar associations have been reported between ejection fraction and serum homocysteine. The current study aims to establish the association between elevated homocysteine level and the extent of myocardial injury measured by cardiac troponin-I and ejection fraction in patients admitted with acute coronary syndrome. These findings would focus on the adverse effects of homocysteine on cardiovascular outcomes in acute coronary syndrome. This study also points towards the fact that certain measures may be planned to control serum homocysteine along with other risk factors in patients of Coronary Artery Disease (CAD) in order to improve the outcomes.
SUBJECTS AND METHODS
This was a cross sectional, open labeled, hospital based study conducted on 200 patients admitted with acute coronary syndrome in the coronary care unit of J N Medical College, AMU, Aligarh, India, during October, 2013 to November, 2014.
Inclusion criteria: Patients admitted with acute coronary syndrome in the coronary care unit.
Exclusion criteria: Patients with cardiomyopathy, congenital heart disease, vulvular heart disease; patients with severe comorbid conditions; patients already taking folic acid, vit. B6, or vit. B12 supplementation.
Informed consent was taken from all patients. A detailed history was taken and a thorough clinical examination was carried out. History was taken regarding risk factors for CAD, previous coronary events and significant family history. Drug history was taken regarding anti hypertensives, statins and and vitamin (B6, B12, Folic acid) supplements. Baseline laboratory investigations like Serum creatinine, lipid profile, RBS, ECG, Echocardiography, were carried out in all patients. Serum homocysteine was measured on fasting sample. Cardiac troponin- I (cTI) was measured after 10 to 12 hours of onset of symptoms. Echocardiography was carried out in all patients and ejection fraction was noted alongwith other necessary parameters.
Statistical Analysis
SPPS version 21 was used for all statistical purposes. All data are expressed as numbers with percentages or mean with standard deviation. Chi square test, student’s t-test, Pearson’s Correlation coefficient, Multiple logistic regression, linear regression, and ANOVA were applied wherever applicable. Level of significance was set at 0.05.
RESULTS
During the study period, two hundred patients of acute coronary syndrome fulfilled the inclusion criteria. Mean age was 56.3±13.2 years, 145 (72.5%) were males and 55 (27.5%) females. Forty seven patients (23%) were known diabetics (43% females). 94 (47%) were smokers. Of the 47 diabetic patients (23%), 24(51%) took oral medications; 12 (25.3%) used insulin. Of the patients with ACS, 62 (31%) had unstable angina, 52 (26%) had NSTEMI and 86 (43%) had STEMI. Patients with STEMI, who gave consent, were thrombolysed whenever indicated (n=54, 46.4%).
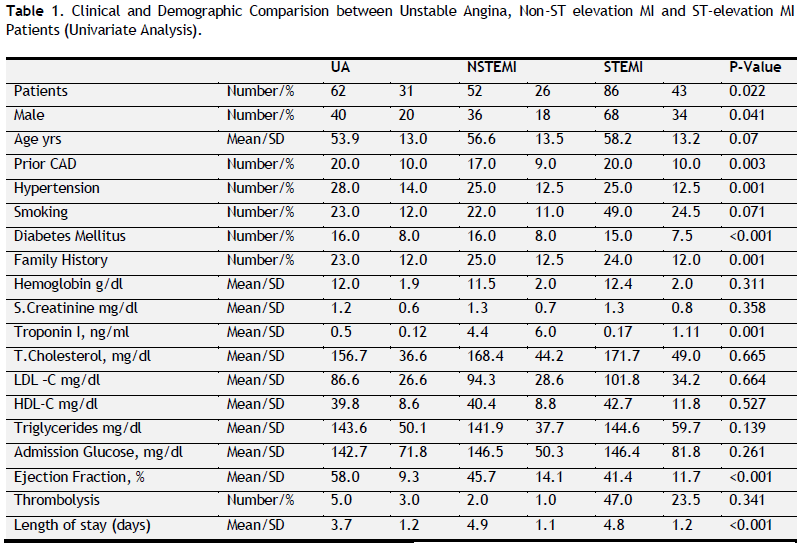 |
Table 1. Clinical and Demographic Comparison between Unstable Angina, Non-ST elevation MI and ST-elevation MI Patients (Univariate Analysis). Click here to view full image |
Table 1 shows a comparison between types of ACS. Among patients presenting with unstable angina, 16 (8%) were diabetic; whereas 15 (7.5%) were diabetic among STEMI patients and 18 (8%) were diabetic among NSTEMI patients. The mean ejection fraction was 58±9.3% among patients of unstable angina; 45.7±14.1% among patients of NSTEMI and 41.4±11.7% among STEMI patients. The average length of stay was longest among patients of NSTEMI (4.9+1.1 days). The average duration of hospital stay was 3.7±1.2 days in patients of UA and 4.8±1.2 days in STEMI patients.
In patients presenting with unstable angina, 20 (10%) were known cases of coronary artery disease, while this number was 17 (9%) and 20 (10%) among patients with NSTEMI and STEMI respectively. 23 (12%) of patients presenting with unstable angina were smokers, whereas, 22 (11%) of NSETMI patients were smokers and 49 (24.5%) of STEMI patients were smokers. This difference was statistically insignificant. The mean cardiac troponin was 0.5±0.12 ng/ml in patients of unstable angina, whereas, it was 4.4±0.17 ng/ml in patients of NSTEMI and 11.7±1.11 ng/ml among patients of STEMI and this finding was statistically significant (p=0.001).
The mean homocysteine level of the study population was 37.65±12.8 μmol/L. Significant positive correlation was found between Serum Troponin-I level and homocysteine level. The values of Pearson’s correlation coefficient was 0.283 which is significant (p<0.001). On applying linear regression, the value of R square was 0.064, and the p value was <0.001 (Fig. 1-2). Also, a positive correlation was found between serum homocysteine levels and ejection fraction. The R square for this relationship was 0.244, with a p value of <0.001 (Fig. 3).Therefore, there was linear positive correlation between Serum Troponin-I level and homocysteine level, as well as between serum homocysteine levels and ejection fraction.
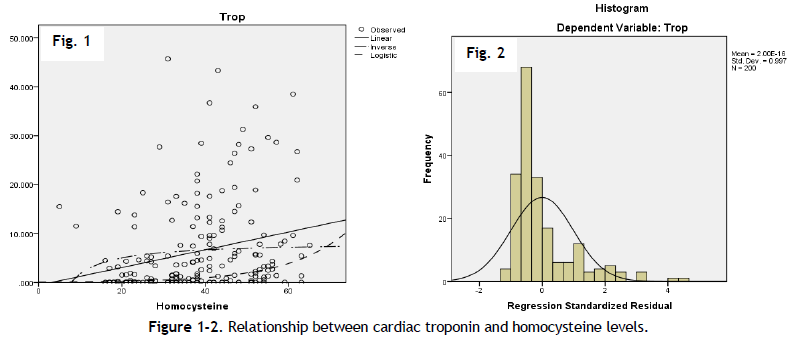 |
Figure 1-2. Relationship between cardiac troponin and homocysteine levels. Click here to view full image |
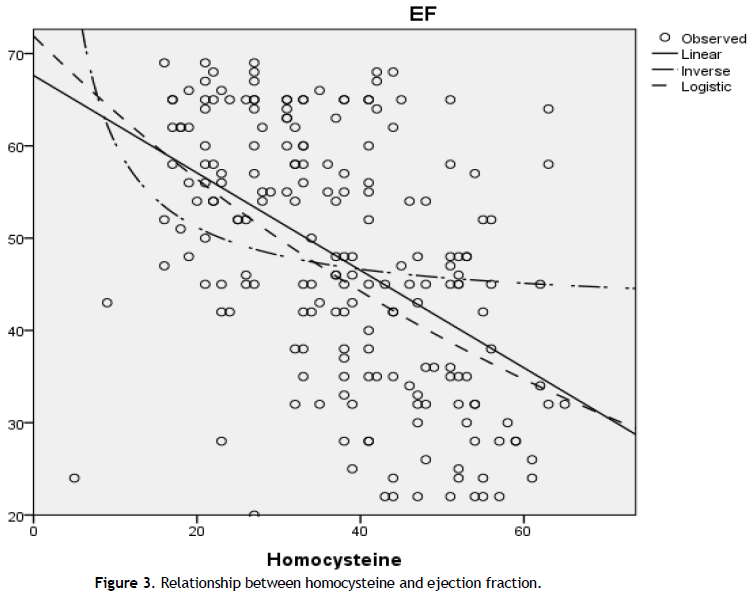 |
Figure 3. Relationship between homocysteine and ejection fraction. Click here to view full image |
DISCUSSION
Elevated levels of homocysteine have been shown to cause increased thrombosis (Allen et al., 2002). There is a paucity of such studies which could demonstrate whether serum homocysteine levels in patients presenting with Acute Coronary Syndrome (ACS) have an association with the degree of myocardial injury. The current study has findings in concert with Obaidi et al., (Al-Obaidi et al., 2000) in which the authors have reported that the rise in cardiac troponin-I was associated with a statistically significant rise in serum homocysteine levels in patients of acute myocardial infarction. In the present study, a positive correlation (p<0.001) was found between serum Troponin-I level and homocysteine levels, which is commensurate with the study of Obaidi et al., (Al-Obaidi et al., 2000).
In the present study, the Troponin- I levels were found to be highest among the patients presenting with ST-elevation myocardial infarction (11.7±11.0 ng/ml). This is similar to previous studies. Takada et al., have reported 1.3±6.5 ng/ml;20.6±34.5 ng/ml and 56.6±57.9 ng/ml in patients with unstable angina, NSTEMI and STEMI respectively (Takada et al., 2012).
It was found in the current study by multiple logistic regression model that increased serum troponin-I levels were not associated with hypertension, family history of premature CAD, dyslipidaemia and obesity (p>0.05). This is in concert with previous studies where no significant correlation has been established between these risk factors and serum homocysteine levels (Alam et al., 2012).
In the present study, we have also observed that there was a strong correlation between serum homocysteine levels and ejection fraction. It may be inferred from the current study that higher the levels of serum homocysteine, lower is the ejection fraction. It is already known that ejection fraction in a patient of acute coronary syndrome denotes the extent of myocardial damage (Klingenheben et al., 2003). Therefore, in the current study, we have demonstrated indirectly that the levels of serum homocysteine correlate with the extent of myocardial damage.
It is known from previous studies, that both serum troponin and ejection fraction correlate with the extent of myocardial necrosis in patients of acute coronary syndrome (Al-Obaidi MK et al.,, 2000; Klingenheben et al., 2003). A higher troponin and a lower ejection fraction also correlate angiographically with the extent of ischemia/infarction (Yuri et al., 2010). Also, both these parameters have been shown earlier to be associated with higher cardiovascular morbidity and mortality in patients admitted with acute coronary syndrome. Our finding of strong association of serum homocysteine with these parameters indirectly highlights the significance of levels of serum homocysteine in the extent of myocardial damage and the immediate outcomes of patients of acute coronary syndrome, as both serum troponin and low ejection fraction are associated with increased mortality and worse outcomes in patients admitted with acute coronary syndrome.
Elevation in serum homocysteine levels may reflect factors such as geographical variations, racial and ethnic differences, genetic causes, inadequate intake of B vitamins and folate (Guthikonda et al., 2006). Cooking habits of populations may also alter the homocysteine levels. Fortification of grain products with folic acid is an important method of keeping homocysteine levels under control. The current study has important repercussions on prevention of mortality and morbidity among patients admitted with acute coronary syndrome. It highlights the significance of homocysteine in acute cardiac states, in contrast to previous studies on homocysteine which have mainly highlighted its role as a long term risk factor of thrombosis. However, further studies are required to ascertain the effect of homocysteine lowering treatment on the extent of myocardial injury during admission for acute coronary syndrome.
CONCLUSION
The current study highlights the fact that elevated serum homocysteine level has a strong correlation with serum cardiac troponin-I and ejection fraction in patients of acute coronary syndrome. Therefore, it may be concluded that serum homocysteine is associated with increased myocardial injury which has been quantified in the current study by serum cardiac troponin-I levels and ejection fraction, which are independent markers of the extent of myocardial damage in patients of acute coronary syndrome.
CONFLICT OF INTEREST
None declared.
REFERENCES
Alam N, Khan HILR, Chowdhury AW, Haque MS, Ali MS, Sabah KMN, Amin MG. Elevated serum homocysteine level has a positive correlation with serum cardiac troponin I in patients with acute myocardial infarction. Bangladesh Med Res Counc Bull. 38, 9-13, 2012.
Allen P. Burke, V. Fonseca, Frank Kolodgie, Arthur Zieske, Louis Fink, Renu Virmani. Increased Serum Homocysteine and Sudden Death Resulting from Coronary Atherosclerosis With Fibrous Plaques. Arterioscler, Thromb, Vasc Biol. 22, 193-1941, 2002.
Al-Obaidi MK, Phillippou H, Stubbs PJ, et al.,. Relationships between homocysteine, Factor VIIa and thrombin generation in acute coronary syndromes. Circulation.101, 372–7, 2000.
Clarke R, Daly L, Robinson K, et al.,. Hyperhomocysteinemia: an independent risk factor for vascular disease. N Engl J Med. 324, 1149–55, 1991.
Eric Boersma, Karen S. Pieper, Ewout W. Steyerberg, Robert G. Wilcox, Wei-Ching Chang, Kerry L. Lee, K. Martijn Akkerhuis, Robert A. Harrington, Jaap W. Deckers, Paul W. Armstrong, A. Michael Lincoff, Robert M. Califf, Eric J. Topol, Maarten L. Simoons. Predictors of Outcome in Patients With Acute Coronary Syndromes Without Persistent ST-Segment Elevation. Circulation. 101, 2557-2567, 2000.
Guthikonda S, Haynes WG. Homocysteine: Role And Implications In Atherosclerosis. Curr Atheroscler Rep. 8, 100-6, 2006.
Harker LA, Ross R, Slichter SJ, Scott CR. Homocystine-induced arteriosclerosis. The role of endothelial cell injury and platelet response in its genesis. J Clin Inves. 58, 731– 41, 1976.
Hayashi T, Honda G, Suzuki K An atherogenic stimulus homocysteine inhibits cofactor activity of thrombomodulin and enhances thrombomodulin expression in human umbilical vein endothelial cells. Blood. 79, 2930–2936, 1992.
Julio Yoshio Takada,, Rogério Bicudo Ramos, Solange Desiree Avakian, Soane Mota dos Santos, José Antonio Franchini Ramires, and Antonio de Pádua Mansur. BNP and Admission Glucose as In-Hospital Mortality Predictors in Non-ST Elevation Myocardial Infarction. The Scient World J. 397915, 2012.
Klingenheben T, Hohnloser SH. Usefulness of risk stratification for future cardiac events in infarct survivors with severely depressed versus near-normal left ventricular function: results from a prospective long-term follow-up study. Ann Noninvasive Electrocardiol. 8, 68–74, 2003.
Nygard O, Nordrehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 337, 230–6, 1997.
Yuri B. Pride, Jennifer L. Giuseffi, , Satishkumar Mohanavelu, Caitlin J. Harrigan, Warren J. Manning, C. Michael Gibson,Evan Appelbaum. Relation Between Infarct Size in ST-Segment Elevation Myocardial Infarction Treated Successfully by Percutaneous Coronary Intervention and Left Ventricular Ejection Fraction Three Months After the Infarct. American J Cardiol. 1016, 4-12, 2010.




 This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.