Mohd Aslam1*, Shadab Ahmad Khan1 , Muhammad Uwais Ashraf1, Anjum Parvez 1, Mohd. Owais2, Juwairia Ashraf3
1Jawahar Lal Nehru Medical College, AMU , Aligarh, UP, India.
2Interdisciplinary Biotechnology Unit, AMU, Aligarh, UP, India.
3AKTC, AMU, Aligarh.
ORIGINAL RESEARCH ARTICLE
Volume 2, Issue 3, Page 154-157, September-December 2014.
Article history
Received: 1 December 2014
Revised: 20 December 2014
Accepted: 25 December 2014
Early view: 31 December 2014
*Author for correspondence
E-mail: [email protected]
Background: In recent years there has been much focus on the existence of generalized endothelial dysfunction in Essential hypertension. Also atherosclerosis, which is a key contributor to Essential hypertension, has been firmly established to be an inflammatory process. High blood pressure [HBP] has been associated with elevated C-reactive protein [CRP], a marker of chronic mild inflammation. This study endeavors to correlate levels of HS-CRP and other co-Variates (Age; BMI; abnormal lipids; blood sugar; Microalbuminuria) and different grades of blood pressure in essential hypertensive patients.
Subject and methods: Sixty newly detected patients of Essential hypertension over a period of one year, categorized into stage 1 or 2 hypertension were recruited in the study. Hs-CRP estimation was done by quantitative ELISA. Other routine investigations like blood sugar, serum lipid profile etc was also done to correlate with various parameters.
Results: HS-CRP levels were consistently found to be elevated in both the stages of hypertension. No significant correlation was observed between levels of HS-CRP and stage of Hypertension (p>0.05). Using Pearson’s Correlation coefficient, HS-CRP levels were found to significantly correlate with TG (P < 0.05), [BS(F) P< 0.001] and age (P < 0.05). Hs-CRP levels are elevated in essential hypertension, but their levels do not correlate significantly with different grades of blood pressure.
Conclusion: Hs-CRP levels are strongly associated with the components of metabolic syndrome (In our study fasting blood sugar and Triglycerides). Microalbuminuria though present in essential hypertension is not significantly associated with the severity of hypertension.
Keywords: HS CRP; Hypertension; Blood Pressure; Lipid Profile; Microalbuminuria.
INTRODUCTION
Patients with elevated arterial pressure and no definable cause are said to have Primary, Essential or Idiopathic hypertension. A variety of complexly interrelated systems in the body: the Central and /or the peripheral Adrenergic, Renal, Hormonal, Vascular have been implicated in the pathogenesis of Essential hypertension. Besides, a number of environmental factors also contribute to the multifactorial causation. Essential hypertension constitutes about 92-94% of all hypertensive patients. Diastolic Hypertension, defined as a diastolic blood pressure of 90 mm Hg or higher, often occurs with a systolic blood pressure of 140 mmHg: so called systolic-diastolic hypertension (Chobanian et al., 2003). When diastolic hypertension occurs with a systolic blood pressure <140 mm Hg it is called isolated diastolic hypertension (IDH) (Pickering, 2003). Isolated systolic hypertension (ISH) is defined as a systolic blood pressure of 140 mmHg and diastolic blood pressure of <90 mm Hg. Borderline hypertension describes BP readings close to the upper limits of the normal range or only slightly elevated. Table 1 shows the JNC-VII classification of blood pressure for adults >18 years.
In recent years there has been much focus on the existence of generalized dysfunction in Essential hypertensive patients, which is a precursor of decreased vascular smooth muscle relaxation. This is attributed to decreased Nitric Oxide availability secondary to impaired production or increased inactivation. Endothelial dysfunction is an important component of essential hypertension, the severity being determined by the stage of hypertension, microalbuminuria, LDL-cholesterol, triglycerides, age and Hs-CRP levels independently (Gupta et al., 2011). Also atherosclerosis, which is a key contributor to Essential hypertension, has been firmly established to be an inflammatory process with local microinflammation in the atheromatous plaque. High blood pressure (HBP) has been associated with elevated C-reactive protein (CRP), a marker of chronic mild inflammation. Hypertension causes increase in pulsatile load and cyclic wall stress on the vasculature, which in turn affects endothelial cell gene expression and function which promote endothelial expression of cytokines and ultimately this lead to increase in inflammatory markers. High sensitivity C-reactive protein (hs CRP) is a hepatically derived pentraxin that plays a key role in innate immune response. It is synthesized primarily in liver in response to IL-6 and IL-1 and has a long plasma half life of up to 20 hours. Individuals without inflammation, usually have CRP levels below 1 g/ml. CRP’s predictive power resides between 1-5 g/ml which is detectable by highly sensitive assays and is known as hs-CRP. There is a good and consistent significant relationship between baseline hs-CRP levels and risk of future cardiovascular disease (stroke, peripheral vascular disease, sudden cardiac death and myocardial infarction) (Danesh, 2007; Kuller et al., 1996). Elevated hs-CRP levels also appear to correlate with softer plaques that are more prone to rupture (Liuzzo, 1994). In fact prospective data suggest that hs-CRP may be a stronger predictor of risk of cardiovascular events than LDL-cholesterol, and it adds prognostic information at all levels of calculated Framingham risk and at all levels of the metabolic syndrome. The study is an attempt to investigate correlation between various inflammatory markers in patients with different grades of Essential Hypertension and to try to correlate them with other co-variates like age, Body Mass Index, lipid profile etc. which might have an important bearing on the conclusions.
SUBJECT AND METHODS
Sixty newly detected patients of Essential hypertension were recruited in the study after taking informed consent from them. The subjects attended Cardiology clinic, Medicine OPD of the Department of Medicine, JN Medical College and Hospital, AMU, Aligarh over a period of one year, and were recruited if they fulfilled the criteria for inclusion. The inclusion criteria was first time detected patient of essential hypertension not on any prior treatment and classified into grade 1 or grade 2 hypertension according to JNC-VII criteria. The exclusion criteria were secondary hypertension including Chronic Kidney Disease; smoking; diabetes mellitus; acute or chronic inflammatory conditions including collagen vascular diseases; acute or chronic infection; familial dyslipidemias; acute coronary syndromes and cerebrovascular accidents; patients on statins or lipid lowering therapy; women on hormone replacement therapy.
Blood Pressure measurement: Strict precautions were taken to ensure proper BP measurement. The patients were asked to rest for at least five minutes. Blood pressure was measured in patients in both the upper extremities in the sitting, supine and standing position (for at least 2 min). Particular note was made for a rise in diastolic B.P. when the patient changed from supine to standing position; a characteristic of essential hypertension while a fall in the absence of antihypertensive medication is suggestive of secondary hypertension. An average of two sitting readings on two different visits was taken before assigning to specific group of JNC-VII classification).
The subjects were asked to report to the endocrinology laboratory after an overnight fast of 10 – 12 hours. Blood samples were collected for plasma glucose, serum lipids, blood urea, serum creatinine, hs-CRP. Other investigations performed were 12 lead Electrocardiogram, chest X-Ray PA view, urine albumin : creatinine ratio (Microalbuminuria), USG abdomen, Color Doppler of renal artery (in selected cases). Hs CRP estimation was done by quantitative Enzyme Linked Immuno Sorbant Assay (ELISA) technique.
RESULTS
Of the 60 essential hypertensive subjects (36 males and 24 females) studied 26 were in stage 1 hypertension (according to JNC VII classification) while the remainder 34 were in stage 2 hypertension (Table 2). Fifteen out of sixty patients (20%) had normal serum Total Cholesterol, LDL-Cholesterol, HDL-Cholesterol and Triglyceride levels. Rest all patients were dyslipidemic with derangement in one, two or all the three components of the lipid profile. Dyslipidemia was defined as: LDL-Cholesterol >130mg% or HDL <40 mg% (Adult Treatment Panel- III Guidelines) or Triglycerides>160mg%. There were 20 dyslipidemics (79.6%) in Stage 1 hypertension and 25(83.3%) in Stage 2 hypertension (Table 3).
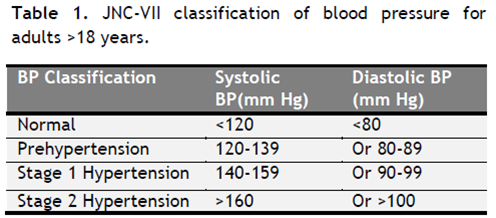 |
Table1. JNC-VII classification of blood pressure for adults >18 years. Click here to view full image |
Microalbuminuria calculated as Urinary albumin: creatinine ratio (UACR) was unrelated to age and Body mass index (p>0.05). The study subjects were divided into three groups according to their UACR values. Group 1 consisted of 44(73.3%) subjects who had UACR values <15 mg/G, while 13.3% (n=8) subjects had borderline microalbuminuria (UACR: 15-30mg/G-Group 2). Groups 3 consisted of an equal number of patients as Group 2, and were classified as having overt microalbuminuria (UACR>30 mg/G). Mean UACR values in Stage 1 hypertension were 17.15 21.55 mg/g as compared to 20.76 28.78mg/g in Stage 2 hypertension, the difference between the two means not being significant (p>0.05) (Table 4).
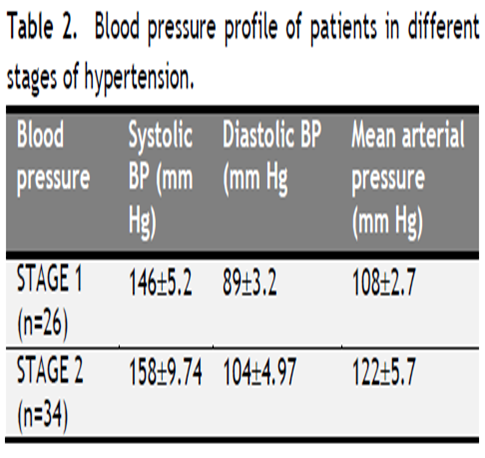 |
Table 2. Blood pressure profile of patients in different stages of hypertension. Click here to view full image |
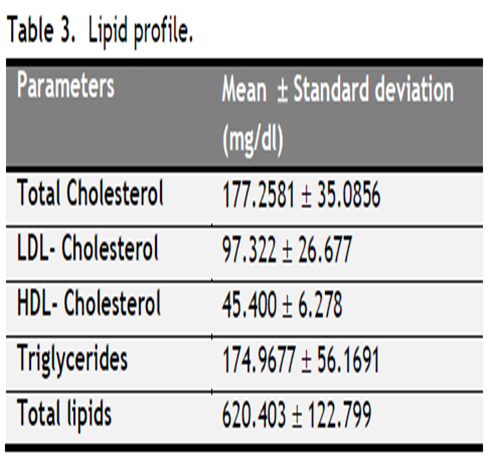 |
Table 3. Lipid profile. Click here to view full image |
 |
Table 4. Urinary microalbuminuria. Click here to view full image |
Only 6 patients had CRP values of less than 2mg/L (10%). Minimum value was 0.337mg/L while maximum was 9.732mg/L. Though females in the study had slightly higher mean values of CRP than the males the difference was not statistically significant (P > 0.05). No significant correlation was observed between levels of Hs-CRP and stage of Hypertension though the levels were elevated in both the stages (Table 5 & 6).
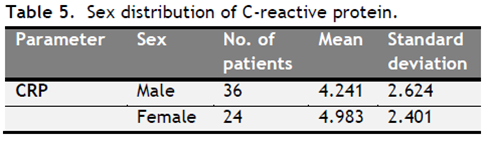 |
Table 5. Sex distribution of C-reactive protein. Click here to view full image |
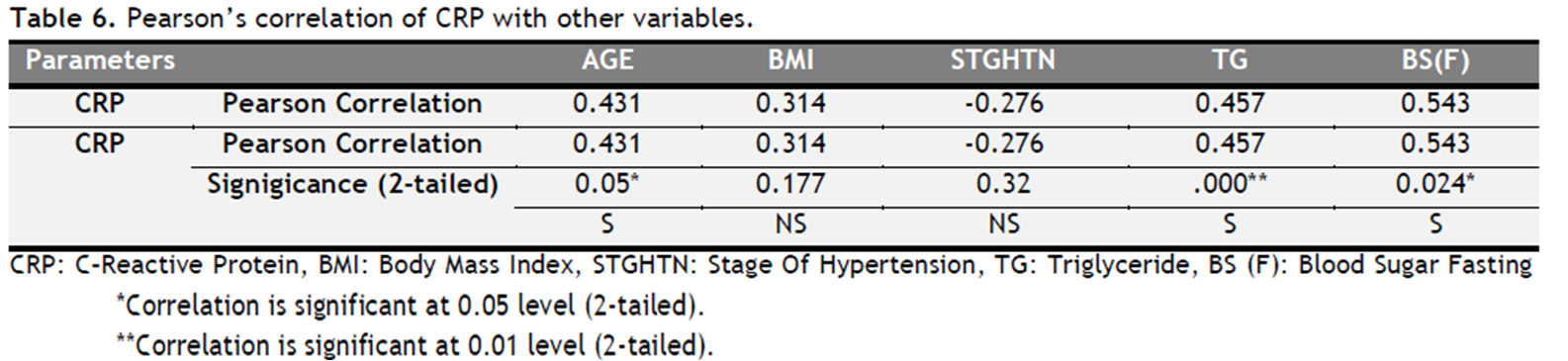 |
Table 6. Pearson’s correlation of CRP with other variables. Click here to view full image |
DISCUSSION
The present study was conducted on newly detected patients of essential hypertension in JN Medical College, AMU, Aligarh, India. The study group comprised of sixty essential hypertensive subjects, 36 males and 24 females categorized into stage 1 or stage 2 hypertension. Most cases were in 50-60 year age group (n=21), while they were more or less equally distributed in other age groups.
Headache was the most common clinical feature, present in 46% cases in stage 1 hypertension and 59 % cases in stage 2 hypertension. Fourteen patients in the study were overweight while eight were obese. There was greater prevalence of Dyslipidemia with increasing BMI. Systolic, Diastolic and mean arterial pressures differed significantly (P < 0.05) between normal and overweight subjects. EKG showed Left Atrial Enlargement (LAE) as the most common isolated abnormality detected in 17%(n=10) of the patients .Fundus examination revealed Hypertensive retinopathy in 18 patients of which 6 had stage 1 and 12 had stage 2 hypertension. There were 20 dyslipidemics (79.6%) in Stage 1 hypertension and 25(83.3%) in Stage 2 hypertension. On comparing microalbuminuria and Hs-CRP values in Dyslipidemics and non- dyslipidemics, a significant difference was found in the levels of Hs-CRP (p <0.05).Urinary microalbuminuria
(Albumin: Creatinine Ratio) was unevenly distributed throughout the study subjects irrespective of the stage of hypertension.
Hs-CRP levels were consistently found to be elevated in both the stages of hypertension in our study. In fact Hs-CRP was found to predict future hypertension in a large study of initially normotensive women, even in subjects with low baseline blood pressure levels (Sesso, 2003). In another study there was greater prevalence of elevated Hs-CRP in patients with systolic or diastolic blood pressure in pre-hypertensive/hypertensive range than people with normal blood pressure (King, 2004). Hs-CRP levels were also found to correlate significantly with fasting Triglyceride and blood sugar levels in our study (P < 0.05). That CRP reflects the Metabolic Syndrome was concluded in Women’s Health Study (Ridker, 2003), a follow-up study involving 14719 American women, which concluded that Hs-CRP is significantly associated with each of the component of the Metabolic Syndrome i.e. fasting Triglycerides, fasting blood sugar, blood pressure, waist circumference and HDL cholesterol. Similar results were obtained by Fransesco and coworkers (Perticone, 2004), who found that Hs-CRP levels were inversely related to vasodilatory response to acetylcholine and glomerular filtration rate. A recent study revealed a graded association between blood pressure and CRP elevation in people with hypertension. Individuals with prehypertension or with shorter duration of hypertension (≤1 Year) had significantly a greater likelihood of CRP elevation in comparison to chronic stage-I or stage-II hypertensives (Shafi, 2010). A similar study among Mongolian population indicated that inflammation and endothelial dysfunction was associated with hypertension and abnormal metabolism, and individuals with co-existence of abnormal metabolism with inflammation and endothelial dysfunction had higher risk of prevalent hypertension (Zhang, 2013).
CONCLUSION
We conclude from the study that:
1. There is a strong association between BMI, hypertension and abnormal lipids.
2. Hs- CRP levels are elevated in essential hypertension, reinforcing the view that hypertension is in part an inflammatory disorder, but their levels does not correlate significantly with different grades of blood pressure.
3. Hs- CRP levels are strongly associated with the components of Metabolic syndrome (in our study hypertension, fasting blood sugar, and Triglycerides though association with HDL cholesterol, LDL and BMI was not significant).
4. There is association between Hs- CRP and fasting blood sugar.
5. Microalbuminuria though present in essential hypertension is not significantly associated with the severity of hypertension.
6. There is no association between Hs-CRP and Microalbuminuria.
CONFLICT OF INTEREST
None declared.
REFERENCES
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ. The seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and treatment of High Blood Pressure; The JNC VII report. JAMA. 289, 2560-72, 2003.
Danesh J, Whincup P, Walker M, Lennon L, Thomson A, Appleby P, Gallimore JR, Pepys MB. Low grade inflammation and coronary heart disease: prospective study and updated meta-analyses. BMJ. 321, 199-204, 2000.
Gupta V, Sachdeva S, Khan AS, Haque SF. Endothelial dysfunction and inflammation in different stages of essential hypertension. Saudi J Kidney Dis Transpl. 22, 97-103, 2011.
King DE, Egan BM, Mainous AG , Geesey ME. Elevation of C-reactive protein in People with Prehypertension. J Clin Hypertens. 6, 562-68, 2004.
Kuller LH, Tracy RP, Shaten J, Meilahn EN. Relation of C-reactive protein and coronary heart disease in the MRFIT nested case-control study. Multiple Risk Factor Intervention Trial. Am J Epidemiol. 144, 537–47, 1996.
Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Rebuzzi AG, Pepys MB, Maseri A. The prognostic value of C-reactive protein and serum amyloid A protein in severe unstable angina disease: prospective study and updated meta-analysis. N Engl J Med. 331, 417-24, 1994.
Perticone F, Maio R, Tripepi G, Zoccali C. Endothelial Dysfunction and Mild Renal Insufficiency in Essential Hypertension. Circulation. 110, 821-825, 2004.
Pickering TJ. Isolated diastolic hypertension. J Clin Hypertension. 5, 411-413, 2003.
Ridker PM, Buring JE, Cook NR, Rifai N. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women. Circulation. 107, 391-7, 2003.
Sesso HD, Buring JE, Rifai N, Blake GJ, Gaziano JM, Ridker PM. C-Reactive Protein and the Risk of Developing Hypertension. JAMA. 290:2945-51, 2003.
Shafi Dar M, Pandith AA, Sameer AS, Sultan M, Yousuf A, Mudassar S. hs-CRP: A potential marker for hypertension in Kashmiri population. Indian J Clin Biochem. 25, 208–212, 2010.
Zhang M, Wang G, Wang A, Tong W, Zhang Y. Association of hypertension with coexistence of abnormal metabolism and inflammation and endothelial dysfunction. Blood Press. 22,151-7, 2013.




 This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.