Md Abrar Hassan1*, Madhura K2, Deedipiya G2
1Department of Physiology, Bhaskar Medical College, Yenkapally, Moinabad, RR (Dist.), AP, India.
2Department of Ophthalmology, Bhaskar Medical College, Yenkapally, Moinabad, RR (Dist.), AP, India.
ORIGINAL RESEARCH ARTICLE
ARTICLE INFORMATION
Article history
Received: 15 December 2013
Revised: 25 December 2013
Accepted: 29 December 2013
Early view: 30 December 2013
*Author for correspondence
E-mail: [email protected]
Keywords:
Ammetropia
Myopia
Hypermetropia
Presbyopia
Astigmatism
Visual acuity
Objectives: To assess the prevalence of refractive errors in women of different age groups.
Subject & Methods: This was a prospective study being carried out on a subject sample size of 150 women, in the age group of 15-60 years divided into 3 groups to assess refractive status in different phases of female life. Group-1 comprising of 50 females in 15-30 years range. Group-2 comprising of 50 females in 31-45 years range. Group-3 comprising of 50 females in 46-60 years range, Subjects were picked up at random from the students, staff and patients attending Bhaskar General Hospital. The subjects were explained about the implication of the study in their own language and a written consent was taken on a prescribed pro forma fulfilling all the norms of ethics.
Results: The subjects were evaluated for visual acuity assessment by Snellen’s chart and Lendolt’s E charts for literates and illiterates respectively. Ocular examination was done for assessing ocular health. Later the subjects were submitted to objective assessment for correction of refractive errors and prescribed spectacles with motivation to use it. Objective assessment is done by retinoscopy under mydriasis to achieve best corrected vision. Data was subjected to Statistical analysis by paired T test .
Conclusion: This study involves women from different backgrounds of life and it was observed that all the 3 age groups of subjects suffered from refractive errors, but the prevalence of Myopia was significantly higher among group-1, consisting of women ranging from 15-30 years, Similarly the incidence and prevalence of Presbyopia was higher amongst the group-2 and group-3 women.
INTRODUCTION
Ammetropia, a condition in which the parallel rays of light will not form a point focus on fovea centralis of the retina resulting in blurring of the vision and asthenopic symptoms like headache, dizziness, photophobia and congestion of eyes is the second most common cause of preventable blindness, covered under WHO’s Vision 2020 program. According to the WHO estimate in 2009 there were 153 million people worldwide living with visual impairment due to uncorrected refractive errors. Thus making the life of patient miserable and affecting the life style. The common ammetropic conditions are myopia, hypermetropia, astigmatism and presbyopia (Gore, 2012). Ammetropia can affect an individual irrespective of his/her age, sex, race or ethnicity. Though, this condition has genetic pre-disposition. It is also affected by the nature of the work and the workplace and the other daily activities of the person i.e., the environmental factors.
Myopia is common when compared to hypermetropia and astigmatism in the younger age groups. There are studies supporting genetics as the cause of refractive error particularly in case of myopia but the present trends is going in favor of visual stress due to too much of close work and due to the excess usage of computers and digital media in day to day life (Sayago et al., 2011). The constant usage of eyes while using computers has led to a group of disorder getting coined under the heading Computer Vision Syndrome which is a common problem in present society and particularly associated with the younger generation due to this changed pattern of life. This technological development has also affected the rural population.
Hypermetropia is the most common condition observed in children. It is usually a continuation of the childhood hypermetropia which has not regressed with time. The problem of this type of refractive error is that it often leads to visual impairment, and is combined with other clinical features like squint and constant headache and hence early recognition is important (Sayago et al., 2011).
Presbyopia is more commonly seen in the aged population caused due to loss of elasticity of the crystalline lens, although changes in the lens’s curvature from continual weakness and loss of power of the ciliary muscles. Although a major portion of the population is still not concerned about their refractive errors and is negligent unless the situation deteriorates to such an extent that it affects their day to day activities. Such gross negligence is mainly noticed in literates and the working population (Salvi et al., 2006).
Another matter of concern is that more than half of the population is not aware of their refractive errors. They are satisfied with whatever visual acuity they are possessing and are able to somewhat manage with their daily chores. This group includes housewives, farm labourers and surprisingly drivers too (Mausumi et al., 2011). On the other hand if we see the female population they are the most affected because there are many misconceptions surrounding the need for glasses, creating a stigma for those who wear them. This affects young women, who are unable to get married because of wearing spectacles. Cosmetic factors play an important role in such situations. The other main reason for discontinuation of spectacle wear in women is due to community pressure. Many women, in a developing country like India, often face social pressure, not only in terms of appearance, but also because of the perception that their children may inherit their visual impairment. Hence they are afraid to disclose their ophthalmological problems to their family. Apart from this the financial constraints also play an important role in affordability of proper spectacles for their refractive state correction. Refractive errors untreated might lead to legal blindness. These groups of disorder of the eye come under preventable causes of legal blindness (Pascolini et al., 2012).
In India, according to a survey conducted in 2007 among the 50+ (age) population, cataract and refractive errors were the major causes of blindness and low vision and control strategies should prioritize them. Most blindness and low vision burden is avoidable (Mausumi et al., 2011). Worldwide refractive errors are one of the priorities of recently launched global initiative for elimination of avoidable blindness–VISION 2020 the right to sight. The refractive error is included under correctable blindness as this can easily be corrected with spectacles (Kamali et al., 1999). The prevalence of myopia, astigmatism, hypermetropia, and anisometropia significantly increased with increasing age. There was no gender difference in prevalence rates in any type of refractive error, though women had a significantly higher rate of hypermetropia than men. Also hypermetropia was significantly higher among those with a higher educational level (Neena et al., 2008). This suggests the negligence of ocular health in women.
Hence the present study is being taken up to bring the latent, correctable cause of blindness especially in women into light as a part of the theme of 2008 for vision 2020.
SUBJECT AND METHODS
Ethical consideration
After obtaining the approval of the Institutional Ethics Committee, the study was carried out between 13-March-2012 and 30-June-2012. The implications of the study were explained to each of the subjects in English and Telugu (local language). A written formal informed consent has also been obtained on a prescribed pro forma fulfilling all the norms of ethics from every individual participant.
During this period a total of 150 women were assessed for visual acuity. The subjects were women belonging to various ethnic groups ranging from 15-60 years selected randomly from the students, staff and patients attending Bhaskar General Hospital. This was a prospective study, conducted in the Department of Ophthalmology in Bhaskar Medical College, Yenkapally, Moinabad, RR (Dist.), AP, India.
Exclusion and inclusion criteria
Women who were not willing to cooperate for visual acuity assessment; suffering with other ocular diseases, squint, infections and pseudophakia in one eye; and below 15 years and above 60 years were excluded from the study. However, all those subjects who were fulfilling the criteria of the basis of the study were included in the study.
The examination of subjects was carried out in the Department of Ophthalmology, Bhaskar General Hospital Moinabad, AP India by a team including an ophthalmologist, an optometrist, a qualified nurse, and the investigator student. The optometrist and the investigator student carried out the visual acuity assessment. The ammetropic women were segregated and subjective and objective assessment of refractive error was carried by ophthalmologist.
All the women were divided into 3 groups comprising of 50 women each; group-1: women of 15-30 yrs, Group-2: women of 31-45 yrs, and group-3: women of 46-60 yrs.
Visual acuity
It was assessed by Snellen’s visual acuity chart by maintaining a distance of 6 meter between the subject and chart under adequate illumination, subjects were asked to read the chart from the topmost letter to the lowest line for individual eye separately.
Unaided and aided visual acuity was tested for those subjects who are already wearing spectacles. Pin-hole test was performed to check the cause of visual loss.
Subjective assessment of the refractive error was carried by ophthalmologist and finally the objective assessment was done in dark room by Retinoscopy and Ophthalmoscopy.
Retinoscopy was done under cycloplegic by using a mydriatic and cycloplegic agent (1% Cyclopentolate eye drops). And 2 drops were instilled in each eye and the subject was made to sit for 1 hour with closed eyes. The examination was done by making the subject sit at 1 meter distance from examiner using streak retinoscopy and the refractive error was assessed by subtracting 1 diopter for cycloplegic used.
Simultaneously, Fundus examination was carried out to check posterior segment for any retinal pathology, as it is the common association of myopia post mydriatic assessment of refractive error was carried on 3rd day at the same place and final prescription for best corrected vision was given to all the subjects.
Parameters assessed
The following parameters were analyzed:
Prevalence of refractive errors.
Correction of refractive error for best corrected visual acuity.
Presenting visual acuity in each eye separately.
Distribution of refractive error as per involvement of eyes.
Statistical analysis
The parameters were analyzed by subjecting the data to paired-‘t’ test for level of significance at 5 % (P value of < 0.05).
RESULT
Prevalence of refractive errors in different groups
It was found that 48% of females were affected with myopia of the total of 150 subjects and hypermetropia accounts for 20% while 50% of elderly group were found to be presbyopic. Astigmatism was seen in 37% of individuals, which is statistically significant (P < 0.05) (Figure 1, 2A-C).
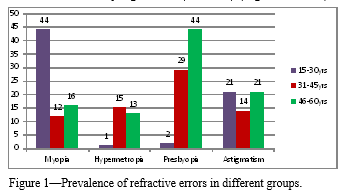 |
Figure 1 Prevalence of refractive errors in different groups. Click here to view full image |
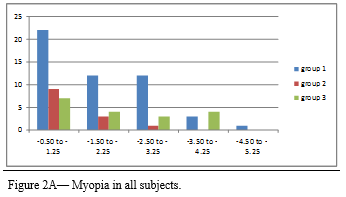 |
Figure 1 Figure 2A Myopia in all subjects. Click here to view full image |
Correction of refractive error for best corrected visual acuity
In group-1, myopia was seen in 88% of subjects while the other refractive errors were negligible (2% hypermetropia). The group-2 subjects showed almost equal predilection to all the 4 types of ammetropic conditions with slight increased trends for presbyopia i.e. 58%, while 24% were myopic, 30% hypermetropics and 28% were astigmatic. The group-3 subjects showed higher incidence of presbyopia with associated distant visual acuity loss due to myopia in 32% of the subjects and hypermetropia in 26% and astigmatism in 42% (Figure 3A-K).
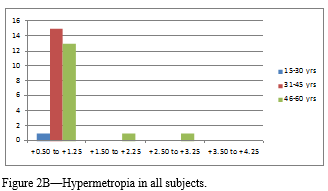 |
Figure 2B Hypermetropia in all subjects Click here to view full image |
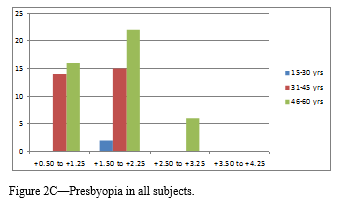 |
Figure 2CPresbyopia in all subjects. Click here to view full image |
Presenting visual acuity in each eye separately
The refractive power calculation and prescription was considered from 0.50 spherical and cylinder glasses and above for best corrected visual acuity. In group-1, 42% of the subjects were corrected in the range of 0.50 to 1.50 spherical and cylindrical correction going up to 2.00, while the highest power prescribed was 5.50 which indicate that the incidence of myopia is high in this age group. While hypermetropia was seen only in 1 subject which was corrected with +1.00 spherical glasses and there were no presbyopia subjects in this group. In group-2, the incidence of refractive errors was inclined to almost all types with 18% myopic subjects getting correction between 0.50 to 1.50 spherical with highest being 3.50 prescribed and hypermetropics incidence was 30% and the correction was between +0.50 to 1.50 spherical. While the presbyopic incidence was highest with 58%, getting correction with upto +2.00 spherical along with the distance vision correction. These subjects accepted cylindrical correction in about 28% cases with +/-0.50 to 1.50 cyl. This effect on refractive state is explained by diminishing accommodation in most of the cases along with lenticular changes. The group-3 subjects showed predilection for presbyopia in 88% and hypermetropia 30% with correction given in the range +0.5 to 1.5 for distance and addition of +2.5 for near in most of the cases. While myopia was recorded in 32% subjects responding to 0.5 to 4.5 sph with astigmatic correction in 20% subjects gave 0.5 to 1.50 cyl. (Figure 3A-K).
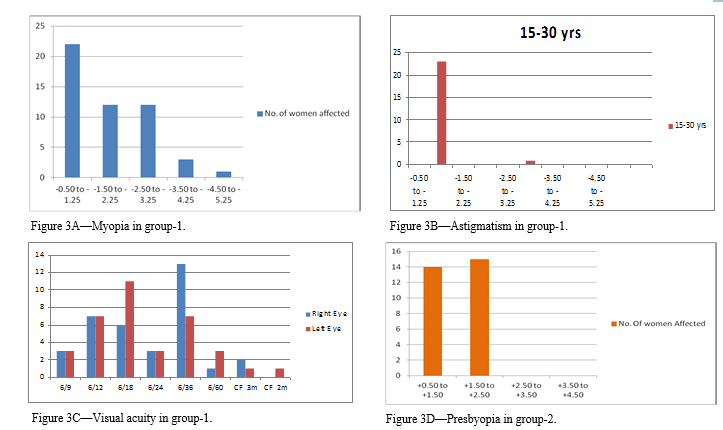 |
Figure 2CFigures describe these are as follow: Figure 3A—Myopia in group-1. Figure 3B—Astigmatism in group-1. Figure 3C—Visual acuity in group-1. Figure 3D—Presbyopia in group-2. Click here to view full image |
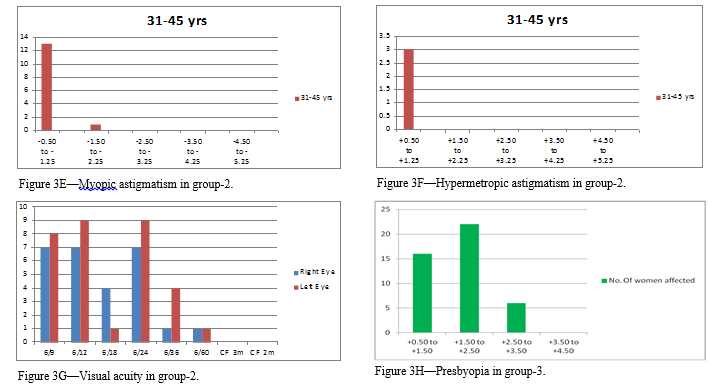 |
Figure 2CFigures describe these are as follow: Figure 3E—Myopic astigmatism in group-2. Figure 3F—Hypermetropic astigmatism in group-2. Figure 3G—Visual acuity in group-2. Figure 3H—Presbyopia in group-3. Click here to view full image |
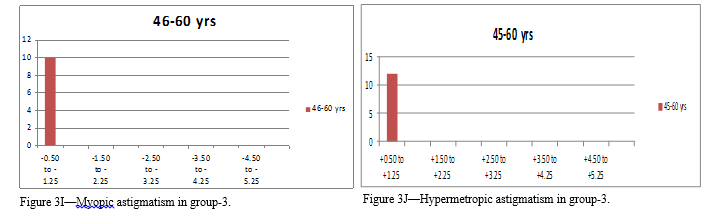 |
Figure 2CFigures describe these are as follow: Figure 3I—Myopic astigmatism in group-3.. Figure 3J—Hypermetropic astigmatism in group-3. Click here to view full image |
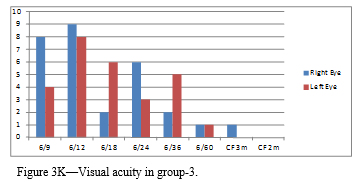 |
Figure KVisual acuity in group-3. Click here to view full image |
Distribution of refractive error as per involvement of eyes.
In group-1, about 365 of subjects were having 6/36 visual acuity but most of the subjects were using correct visual acuity glasses except for 3 subject who were having 6/9 were new entrants. In group-2, about 285 subjects were having visual acuity of 6/9 and 6/12 and were ignorant about the refractive error while this group subject were also ignorant of presbyopic status and were corrected during the study. In group-3, most of the subjects were corrected for visual acuity disturbance as the cause of blindness was cataract in most of the cases and these were treated by pseudophakic implantation of IOL while the remaining were having bifocal visual loss and that was corrected with distance and near correction. Only 8% subjects were suffering with severe visual loss with visual acuity at 6/60 to less than CF 3 meters (Figure 3A-K).
Distribution of refractive error as per involvement of eyes.
Another parameter in this study was accommodation convergence reading which was assessed by using RAF rule the normal accommodation is 20 mm and convergence is 20 mm. There was significant variation in these values in group 2 and 3. In group-1 only 8% subjects were having accommodation and convergence above 20 mm which was seen in individual with hypermetropia due to generalized weakness. In group-2, the accommodation was above 20 mm in 66% of subject and the convergence was high in 40% subject this is the reason for early presbyopia in early thirties and could be due to general weakness and anaemia. In group-3, the accommodation convergence anomalies was highest ranging about 88% and 84 % this could be due to loss of accommodation after surgical procedure and also weakness of extra ocular muscle could be the reason for decreased convergence (Figure 3A-K).
DISCUSSION
This study is done to evaluate the ammetropia in female population attending the out-patient Department of Bhaskar Medical College. The subjects were divided into three groups based on the age. It was found that 48% of females were affected with myopia of the total of 150 subjects and hypermetropia accounts for 20% while 50% of elderly group were found to be presbyopic. Astigmatism was seen in 37% of individuals, which is statistically significant (Figure 1, 2A-C).
The refractive status in each group was different and the correction for the best visual acuity was also variable. Myopia was seen in 88% of subjects in the group-1 while the other refractive errors were negligible (2% Hypermetropia) and there was a significant astigmatic association with myopia seen in 42% of the subjects. This could be attributed to ocular strain and stressful life due to academic obligation apart from excess usage of computer in this group. The group-2 subjects showed almost equal predilection to all the 4 types of ammetropic conditions with slight increased trends for presbyopia, myopic, hypermetropics and astigmatic (Figure 3A-K). This could be explained by the fall in accommodation, convergence ratio at this age thus favouring presbyopia in correlation to the previous studies carried out by Nirmalan et al. (2006) conducted a population-based assessment of presbyopia in the state of Andhra Pradesh, south India: the Andhra Pradesh Eye Disease Study that showed that the female sex (OR: 1.4, 95% CI: 1.1-1.8) were more associated with presbyopia. The group-3 subjects showed higher incidence of presbyopia with associated distant visual acuity loss due to myopia in 32% of the subjects and hypermetropia in 26% and astigmatism in 42%. This change in refractive error can be explained that it is due to nuclear sclerosis and cortical cataract leading to index type of myopia and hypermetropia. While the increase in astigmatic cases was seen in both eyes pseudophakic subjects correlating with the study carried out by Patel et al. (2006) which concluded that the high prevalence of presbyopia, and increased aging of the population in developing countries, suggests that the World Health Organization’s Vision 2020 refraction agenda should place greater emphasis on presbyopia (Ilesh et al., 2009). Refractive power calculation and prescription was considered from 0.50 spherical and cylinder glasses and above for best corrected visual acuity.
The refractive power calculation and prescription was considered from 0.50 spherical and cylinder glasses and above for best corrected visual acuity. This effect on refractive state is explained by diminishing accommodation in most of the cases along with lenticular changes. The changes can be attributed to post-operative changes which develop due to pseudophakic changes and scarring effect on the cornea leading to astigmatism while the high incidence of presbyopia is due to loss of accommodation. Though uniocular presbyopia eyes are excluded for the study but this age group has more cases of lenticular opacities, which is creating index type of ammetropic.
The main aim of this study is to project the ignorance of refractive errors in the female population and this was confirmed by visual acuity. This parameter showed that most of the middle aged women were negligent and ignorant about their visual loss because of the family obligation. While the younger group which forms literate population were aware of visual loss and were corrected with suitable prescription, only the early visual acuity loss was not corrected. The older subject has significant number of corrected visual acuity as most of them underwent surgeries and were comfortable with post operative results.
Another parameter in this study was accommodation convergence reading which was assessed by using RAF rule the normal accommodation is 20 mm and convergence is 20 mm there was significant variation in these values in group 2 and 3.
CONCLUSION
This study involves women from different backgrounds of life and this is observed that all the 3 age groups of subjects suffered from refractive errors, but the prevalence of myopia was significantly higher among group-1, consisting of women ranging from 15-30 years. Similarly the incidence and prevalence of presbyopia was higher amongst the group-2 and group-3 women. Astigmatism and presbyopia was highest in group-3. Of all the affected subjects there were more number of uncorrected ammetropic women in groups-2 and 3 supporting the evidence for negligence and ignorance of ocular health problems particularly in women. The accommodation and convergence anomalies are indicative of general health of these subjects. The magnitude of refractive errors is less in the illiterate and unemployed population when compared to the educated and working women.
REFERENCES
Gore VS. Prevalence of refractive error in illiterate population in Navi Mumbai, Maharastra, India. Int J Bioinform Res, 4, 263-264, 2012.
Ilesh Patel, Sheila Wes. Gender differences in presbyopia: Community Eye Health. 22, 27, 2009.
Neena J, Rachel J, Praveen V, Murthy GV. Rapid Assessment of avoidable blindness India study group. PLoS One. 3, e2867, 2008.
Kamali A, Whitworth JA, Ruberantwari A, Mulwanyi F, Acakara M, Dolin P. Causes and prevalence of non-vision impairing ocular conditions among a rural adult population in SW Uganda. Ophthalmic Epidemiol. 6, 41–48, 1999.
Mausumi Basu, Palash Das, Ranabir Pal, Sumit Kar, Vikas K Desai, Kavishwar A. Spectrum of visual impairment among urban female school students of Surat. Indian J Ophthalmol. 59, 475–479, 2011.
Nirmalan PK, Krishnaiah S, Shamanna BR, Rao GN, Thomas R. A population-based assessment of presbyopia in the state of Andhra Pradesh, south India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci. 47, 2324–2328.
Pascolini D, Mariotti SPM. Global estimates of visual impairment: 2010. Br J Ophthalmol. 96, 614-618, 2012.
Patel I, Munoz B, Burke AG, Kayongoya A, McHiwa W, Schwarzwalder AW, West SK. Impact of presbyopia on quality of life in a rural African setting. Ophthalmology. 113, 728–34, 2006.
Salvi SM, Akhtar S, Currie Z. Ageing changes in the eye. Postgrad Med J. 82, 581–587, 2006.
Sayago S, Sloan D, Blat J. Everyday use of computer mediated communication tools and its evolution over time: an ethnographical study with older people. Interacting with Computers. 23, 543-554, 2011.




 This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.